Your Child's Condition
Complex Conditions
Pediatric Plastic Surgery
Surgery in a newborn baby
 Newborn babies frequently require surgery. To deal with newborn babies is a different ball game altogether. It requires a team effort with the pediatric surgeon, anaesthesiologist, neonatologist, pediatrician, and perinatologist,
Newborn babies frequently require surgery. To deal with newborn babies is a different ball game altogether. It requires a team effort with the pediatric surgeon, anaesthesiologist, neonatologist, pediatrician, and perinatologist,
Outcome of the disease depends upon the degree of prematurity, birth weight, presence of any associated anomalies, the competence of the NICU team and the skill and judgement of the pediatric surgeon. It requires patience, skill and an ability to imagine future life with the changes that the surgery will cause.
Please ask for a counseling session if you are not completely sure about what has been explained to you. Each condition is briefly explained in the various sections on this page. You can also search for your baby’s condition in the search bar. If there are any doubts, please write to us at jivichildcare2019@gmail.com. We would be happy to provide further information.
Pediatric Chest and Airway Surgery

1. Empyema Thoracis
Empyema is a condition where pus collects in the chest
Empyema usually develops following pneumonia. Tuberculosis is another cause of Empyema especially in India
Empyema is usually suspected when a severe bout of pneumonia does not improve with treatment. Children usually show symptoms of being generally unwell with a high temperature with difficulty in breathing.
If Empyema is suspected, chest Xrays are done followed by a Ultrasonography of the chest to see for the location, quantity of pus.. CT scan may be advised to look for any structural problems and extent of disease in the lung
Empyema is treated depending on the extent of the disease by the following 3 treatments.
- Chest tube insertion alone to drain the pus or in an emergency if there is too much breathlessness.
- Minimally invasive surgery – VATS (Video assisted thoracoscopic surgery) wherein a telescope is inserted into the chest cavity and all the pus is removed under vision. The surgery is completed with 2 or 3 small (half an inch) cuts.This is the commonest treatment for Empyema.
- Thoracotomy and decortication – Open large incision surgery on the chest done in late stage empyema or if during VATS , the surgeon decides that it is better for the patient.
The outlook for children with empyema is usually good once it has been diagnosed early and treated promptly. Long term lung damage is rare.
2. Congenital Lung lesions
There is some abnormal lung tissue /mass that is present since birth which sometimes causes problems in breathing
They include CCAM (congenital cystadenomatoid malformation), CLE (congenital lobar emphysema), BPS (bronchopulmonary sequestration)
This may be a single cyst or a collection of multiple cysts present in the lung at birth or may be apparent anytime after birth. If it is interfering with normal breathing, surgery may be required in the newborn period.
But otherwise, these masses can be kept under close observation and they may disappear, or may be required to be removed surgically at a later date. Sometimes these may get infected. Then they have to be removed after the infection is under control.
In this condition, a lobe of the lung enlarges sue to abnormal lung trapping and causes the other lobes to collapse, pushing the heart to one side. This abnormal lobe needs to be surgically removed, more often than not in an emergency setting.
BPS is an extra nonfunctioning part of the lung with an abnormal blood supply by an artery from the abdomen. It needs surgical removal.
3. Tracheo-esophageal fistula
This is a condition in which there is a connection between the esophagus (food pipe) and the trachea( wind pipe) and the continuity of the esophagus is disrupted.
It requires surgical correction, in which the connection between the esophagus and trachea is divided and the esophagus is reconstructed.
If this is not possible due to a large gap between the disrupted ends of the esophagus, the end of the upper esophagus is brought out to through the neck to drain the swallowed saliva and a tube is placed in the stomach to provide nutrition.
Tests are required to detect any associated defects in the other systems like heart, brain, kidneys which have a bearing on the outcome.The connection of the trachea to the esophagus causes problems like pneumonia/respiratory infections, which adversely affect the outcome of surgery.
4. Diaphragmatic hernia (CDH)
A defect in the diaphragm ( internal partition between the chest cavity and abdominal cavity) causes the abdominal contents like intestines, liver, spleen kidneys etc. to migrate into the chest resulting in a diaphragmatic hernia.
The lungs maybe underdeveloped in this condition causing difficulties in breathing after birth.
A few tests have to be done after birth to assess the condition of the heart and lungs. Breathing has to be stabilized either by giving oxygen or by a ventilator. The pressure in the lung has to be brought down to near normal by medications. After this, surgical correction is done
Surgery may be performed through the chest or through the abdomen. It may be performed by an open method or endoscopically depending on the condition of the baby.
5. Airway stenosis
Airway Stenosis is a constriction or narrowing in the windpipe. It can be present at birth (congenital) or acquired due to prolonged ventilation or caused by an injury. Commonest is a subglottic stenosis which is a narrowing present just below the vocal cords.
Symptoms of stenosis can be present shortly after birth or develop after an injury to the trachea. Symptoms include: noisy breathing, wheezing, recurrent pneumonia, inability to wean off ventilator etc
A suspicion of the narrowing is confirmed by performing bronchoscopy. Lower degrees of stenosis just need some time to resolve, but critical reduction in the lumen of the airway/severe stenosis may require urgent tracheostomy or reconstructive airway surgery .
It is a complex surgery, which will require a check bronchoscopy a few times to see resolution/healing or any complication. Most of all, it takes time and patience, but most patients do well if they have no other morbidities.
6. Foreign body in airway
FOREIGN BODIES IN THE AIRWAY ARE A MEDICAL EMERGENCY AND REQUIRE IMMEDIATE ATTENTION.
Foreign body aspiration is when an object is inhaled and becomes lodged in a child’s airway or lungs. Children often examine even non-food substances with their mouth. Most common objects include peanuts, seeds, nuts, small pieces of toys.
Most common symptoms:
- Choking or gagging
- Wheezing (a whistling sound usually made when the child breathes out)
- Stridor (a high-pitched sound usually heard when the child breathes in)
Rigid Bronchoscopy is the standard treatment of choice to remove a foreign object from the airway. Sometimes , in an emergency, if oxygenation is very poor, an emergency tracheostomy or open chest surgery may be needed to extract a difficult foreign body owing to its shape or size.
7. Choanal atresia
It is a condition in which one or both nostrils/nasal passages are blocked since birth either by cartilage or by bone
Newborn babies are nose breathers, so blockage of both nostrils leads to severe decrease in taking oxygen in the body, which leads to a crisis. Hence this needs to be treated immediately. If only one nostril is blocked, surgery may not be needed immediately
A procedure is required in which the cartilage or bone blocking the nasal passages is removed and a passge is created. This needs to be stented by a tube for a few days to prevent reblocking.
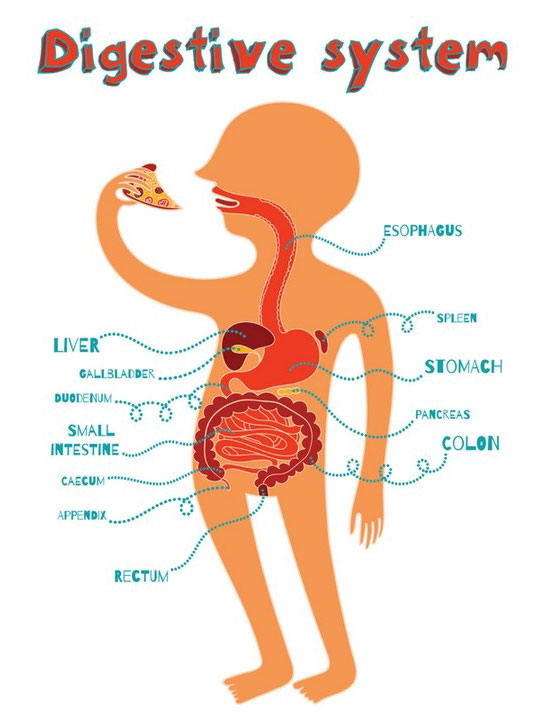
Pediatric Gastrointestinal conditions
- Necrotisingenterocolitis
- Malrotation
- Gastroesophageal reflux
- Anorectal Malformation
- Omphalocele/Exomphalos
- Gastroschisis
- Idiopathic Hypertrophic Pyloric Stenosis(IHPS)
- Duodenal atresia
- Small bowel atresia
- Meconium ileus
- Hirschsprung disease
- Meckel’s Diverticulum
- Intussusception
- Alimentary tract duplications
- Mesenteric and Omental Cysts
- Rectal polyps
- Appendicitis
1. Necrotisingenterocolitis
Severe inflammation/infection of the bowel is called NEC. It causes blood in stools. It usually causes a temporary intolerance of milk feeds but at its worse the bowel may be so damaged that parts of it actually die. NEC may affect just a small part of the bowel or, on occasions, the whole bowel may be affected.
It has a variable course ranging from feed intolerance and abdominal distension (swelling) to a sudden collapse of a baby who had previously been relatively well.
NEC is a condition that is almost exclusively confined to newborn babies in the first days to weeks after birth. It is much more common in premature infants and particularly those who have a lot of other medical problems
If a baby is suspected to be developing NEC or has definite evidence of NEC the following treatments may be started:
Stopping milk feeds – resting the bowel appears to help the bowel recover. Starting antibiotics to treat any infection – bacteria seem to play some part in the development of NEC and therefore antibiotics may help settle the process down. Intravenous feeding is required to keep the baby nourished while milk feeds cannot be given.
If the baby becomes generally unwell a number of other treatments may be necessary, for example, help with breathing, medication to help blood pressure.
X-rays and blood tests will be done to both confirm the diagnosis and monitor the response to treatment. Many babies who develop NEC recover with these ‘medical’ treatments.
However if an area of bowel dies or there is a perforation (hole) of the bowel further treatment may be necessary
Insertion of drain – A drain can be inserted into the baby’s abdomen to allow any free air or fluid to drain out. This is often performed in the first instance especially if the baby is too unwell for an operation, however an operation may still be necessary at a later point.
Laparotomy – An operation under general anaesthetic. The surgeon will aim to remove the part of bowel that has died and rejoin the two ends together (resection and anastomosis). Sometimes it may be very difficult to operate in the abdomen so a stoma (bowel opening onto the abdominal surface) maybe created. In this case the baby will need a further operation to rejoin the bowel together.
Your baby will:
- need help with breathing so will be connected to a ventilator.
- be closely monitored and will be attached to various monitors.
- be intravenously fed. A long line will probably be needed for intravenous feeding.
- be given pain relief as necessary.
- need blood products and other medications.
Most babies who recover from NEC do not have further problems; but future problems are possible especially if there has been bowel perforation. These include:
- NEC may recur
- the wound may become infected or break down.
- the bowel may narrow due to scar tissue either caused by damage to the bowel or at the operation site. This is called a stricture. If this occurs another operation will be necessary to remove this piece of bowel.
- Sometimes if a lot of bowel has been removed this may cause problems with food absorption and therefore growth.
2. Malrotation
It is the malposition of bowel which gives rise to an abnormal twisting of the bowel which results in obstruction and later on gangrene (death) of intestines
It needs to be surgically treated. The intestine has to be derotated and fixed. If there is some segment of gangrenous intestine, it needs to be removed and the healthy edges rejoined.
3. Gastroesophageal reflux
This is the regurgitation of milk feeds because of laxity of the junction between the food pipe and the stomach. It is diagnosed by a dye swallow study.
Usually this improves with age . The babies are given some medicines to improve gastric emptying. A different position of feeding is instituted.
Some babies may have recurrent chest infections due to the ingested feeds going doing the wind pipe. This requies a surgery to tighten the junction between the food pipe and the stomach. This operation is called fundoplication. The baby may also require a tube placed directly into the stomach from the abdominal wall (gastrostomy tube) for direct feeding into the stomach.
4. Anorectal Malformation
Anorectal malformation is a term used to describe several types of anomalies. The anus (which is the opening in the bottom through which stool passes through) and the rectum (which is the part of bowel immediately above the anus) have not developed properly. The baby may be born with:
- No anal (bottom) opening at all
- An ectopic anus (small opening in the wrong place)
- Anal stenosis (narrowed opening of the bottom)
We usually classify them as “high” or “low” anomalies depending on the gap between the bowel and the skin. The bowel may be joined by a fistula (communicating tube) to another structure such as the urinary tract or the reproductive system.
Most babies will have otherwise of developed normally. However there can be other problems with the development of other systems such as the kidneys, heart, spine and oesophagus (VATER syndrome). Other tests such as x-rays and ultrasound scans will be done in the first few days to exclude these.
Feeds, if started, will be stopped and a nasogastric tube (a tube through the nose down to the stomach) will be passed. This enables us to keep the stomach empty so the baby does not vomit and the baby will be given fluid through a drip sited in one of its veins. An X-ray will be taken after 24 hours of age (this allows time for swallowed air to travel through the bowel) to determine whether the anomaly is:
- ‘Low’ – if the bowel is present just under the skin
- ‘High’ – if the bowel ends up higher within the baby’s tummy
Treatment will vary depending on the classification but usually an operation will be necessary.
An operation, called an anoplasty, will be performed that will expose the anus under the skin. This is a relatively minor operation and the baby should be able to feed and pass stool within a day or so of the operation.
The baby will require a temporary colostomy initially. This means bringing an end of the bowel out on to the surface of the tummy so the baby will pass stool into a bag rather than through the anus.
The baby will have the colostomy for several weeks/months until a more complicated operation is performed to create a new bottom for your baby.
Most children are unable to develop normal bowel control but there are ways that we can help to achieve this through a bowel management program. With modern techniques it is usually possible for children to be clean most of the time. This will be discussed further throughout long-term outpatient follow up.
5. Omphalocele/Exomphalos
Exomphalos is a weakness of the baby’s abdominal wall where the umbilical cord joins it. This weakness allows the abdominal contents, mainly the bowel and the liver to protrude outside the abdominal cavity where they are contained in a loose sac that surrounds the umbilical cord..
The cause of this condition is unknown and is a rare problem occurring in about 1 in 5000 pregnancies. About half of all babies with Exomphalos will have problems affecting other body systems. Most commonly affected are the heart, lungs, and kidneys.
After the baby is born, the sac will be wrapped in a protective film to reduce heat and fluid loss. A drip will be placed into a small vein so that intravenous fluids can be given. A tube will be passed through baby’s nose into the stomach to drain away the green fluid (bile) that collects in the stomach. This lessens the risk of your baby vomiting and reduces discomfort.
The size of the sac and its contents can vary greatly from being very small to very large. It is therefore impossible to say exactly what type of operation is required for Exomphalos until your baby is born and the actual size can be seen. However there are a number of different treatments any of which can be used depending upon the size of the Exomphalos. These are:-
Primary repair – If small, it is possible in one operation to replace the Exomphalos inside the abdominal cavity and repair the muscles the skin.
Staged repair – If the Exomphalos is very large, the baby would require an initial operation to construct a temporary envelope of plastic sheeting (silo) outside the abdomen. The silo would then be made smaller over a period of about ten to fourteen days, so that the abdominal contents are gradually pushed back inside the abdomen..A final operation is necessary to completely replace the abdominal contents and repair the muscles and skin..
The surgeon may opt just to close the skin of the abdomen over the Exomphalos and not to repair the muscles and a further operation will be needed to repair the hernia at about three years of age.
Conservative treatment – If the Exomphalos is very large it may not be possible to close it until your baby is older and the size of the abdominal cavity has grown.
6. Gastroschisis
Gastroschisis is the condition in which a baby has a small hole in the front of the abdomen, just to the side of the umbilical cord, through which some of the bowel (intestine) is protruding. This bowel is easily visible on the ultrasound scan.
This is a rare problem, which occurs in around one in every 3000 births, and there is currently no known cause.
Following delivery the bowel will be wrapped in a protective film to reduce heat and fluid loss. A drip will be placed into a small vein so that intravenous fluids can be given, as your baby will not be able to feed in the normal way. A tube will be passed through your baby’s nose into the stomach to drain away the bile (green fluid) that collects here. This lessens the risk of vomiting and reduces discomfort.
Shortly after delivery we may either surgically place the bowel back in the abdominal cavity or we may slide the intestine into a plastic bag (pre-formed silo) where it will remain for a few days. During this time the intestine will be gently squeezed back inside the baby’s abdomen. Once the intestine is all back in, the bag will be removed and dressings placed over the hole. The hole will then heal up over the next 2 weeks.
In a small number of babies the Gastroschisis is complicated by further problems with the bowel that are not normally detected before the baby is born. The blood supply to the bowel is sometimes interrupted resulting in parts of the bowel being irreversibly damaged or missing. This is known as short bowel syndrome. It could mean long term hospitalisation and drip feeding.
7. Idiopathic Hypertrophic Pyloric Stenosis(IHPS)
Gastroschisis is the condition in which a baby has a small hole in the front of the abdomen, just to the side of the umbilical cord, through which some of the bowel (intestine) is protruding. This bowel is easily visible on the ultrasound scan.
This is a rare problem, which occurs in around one in every 3000 births, and there is currently no known cause.
It is an obstruction at the outlet of the stomach where the feed would go from the stomach to the small intestine. It is due to the enlargement of a muscle at that junction
Baby may have projectile vomiting of milk or curds and is very hungry after that. One may see visible movement of the stomach in the upper abdomen (tummy)
The treatment is by an operation in which the overgrown muscle is divided.
8. Duodenal atresia
Duodenal atresia occurs in the duodenum and causes a blockage. The duodenum is the bowel adjoining the stomach. Atresia means gap. Occasionally there may not be a complete atresia but a partial narrowing (stenosis) instead.
There is no known cause for this, but it is believed to have occurred sometime during the early weeks of pregnancy.
The diagnosis is made by seeing two fluid filled areas in the baby’s abdomen which are the dilated stomach and duodenum. This is referred to as the ‘double bubble’ of duodenal atresia. This may have been detected on an antenatal scan or may not be detected until after the delivery when the baby starts to vomit.
Babies with duodenal atresia vomit soon after birth and the vomit is usually bile-stained (green), after which:
- milk feeds, if started, will be stopped.
- a tube will be passed through the nose into the stomach to drain away any fluid and air collecting in the stomach.
- fluids will be given through a vein (drip).
An X-ray of the baby’s tummy will confirm the diagnosis. Very occasionally it maybe necessary for your baby to have another X-ray to confirm the diagnosis.
An operation will be necessary in the first few days of life.
The surgery is carried out through a small incision on the baby’s abdomen. The two ends of the duodenum are joined together and the incision closed again.
Your baby will be kept comfortable with pain killers as required.
In babies with this condition it usually takes two weeks before the bowel is able to tolerate milk feeds, although in some babies it may be longer than this.
Milk feeds will be slowly introduced and increased, as the baby is able to tolerate them. Once recovery has begun the baby should be able to feed normally, either by bottle or breast.
Usually there are no long term effects of duodenal atresia.
However, following an operation, there is always a small risk of future obstruction occurring. If your baby has a bilious vomit or a distended abdomen medical advice should be sought.
9. Small bowel atresia
The small bowel is the section of bowel between the stomach and the large bowel (colon). It is about 300cm long in a newborn baby at full term and its function is to absorb food.
An atresia is a gap in the bowel causing a complete blockage (obstruction) of the bowel. It occurs in about 1 in 5000 babies.
Babies can have over half the bowel missing without there being much effect on milk (or later, food) absorption. However in some babies there is so much bowel missing that special feeding is needed. This is known as short bowel syndrome. It could mean long term hospitalisation and drip feeding. Sadly many of these babies do not survive.
Babies with small bowel atresia vomit soon after birth and the vomit is bile-stained (green), after which:
- Milk feeds will be stopped.
- A tube will be passed through the nose into the stomach to drain away any fluid and air collecting in it.
- Fluids will be given through a vein (drip).
An operation will be necessary in the first few days of life. The ends of the atresia are cut away and the bowel joined back together.
After the operation
Small amounts of milk are usually started after 5 or 6 days and gradually increased.. If the section of bowel above the blockage has become very dilated before birth it may take longer to start working and so some babies need to stay longer.
During this time the baby will need drip feeds (Parenteral Nutrition) through a long line.
Milk feeds will be slowly introduced and increased, as the baby is able to tolerate them. Once recovery has begun the baby should be able to feed normally, either by bottle or breast.
10. Meconium ileus
Meconium Ileus (MI) is a condition where the content of the baby’s bowel (meconium) is extremely sticky and causes the bowel to be blocked at birth. In most cases the bowel itself is complete and intact but it is just the inside that is blocked.
In some cases there has been a twist of the bowel before birth, which has caused the bowel to be blind ending (an atresia).
There is normally a delay in your baby passing meconium (black sticky stool normally passed within 24 hours of delivery) and your baby may also be reluctant to feed and may vomit a green fluid called bile which would normally pass through the bowel.
Some babies present at delivery with a distended abdomen and may be unwell due to infection around the bowel.
- Milk feeds will be stopped
- A tube will be passed through your baby’s nose into the stomach to drain away the bile (green fluid) that collects here. This reduces the risk of your baby vomiting and reduces discomfort.
- Your baby will be given fluid through a drip sited in a vein
- Antibiotics may be started to treat any infection
The effects of Meconium Ileus vary from baby to baby. In some babies it is possible to dissolve the sticky meconium by injecting a fluid via a soft tube into the baby’s bottom (enema) during the course of an x-ray.
In some babies there may be associated complications which means that an operation is necessary. Occasionally it is necessary to bring the bowel out onto the surface (a stoma) as a temporary treatment for a few weeks.
The diagnosis is usually suggested on x-rays of the abdomen.
This is a fairly common genetic condition.
Babies who have CF may have very sticky poo causing plugs. Exactly how CF affects the individual child in other ways varies greatly. Children with CF can have frequent chest infections, this is because they have thick mucus in their lungs which they may find difficult to cough up. They may also have problems with digestion and have to take medicine with food.
It is difficult to predict how the condition will progress but early treatment is believed to be beneficial to the long term outlook of the individual child.
Milk feeds will be started slowly over the first few days. This may be your own breast milk or a formula feed.
If your baby has a stoma this will be closed a few weeks or months after your baby has gone home. Following an operation there is always a small risk of future obstruction occurring.
If your baby has a bilious vomit or a distended abdomen medical advice should be sought.
11. Hirschsprung disease
Hirschsprung’s disease (HD) is a rare condition which affects the nerve cells (known as ganglion cells) of the bowel.The ganglion cells control the muscles of the bowel, and these muscles push along the bowel contents.
There is no known cause for HD, although it can run in families.
HD affects the rectum and a variable length of the large bowel above it. This length is usually a few centimetres but sometimes may affect the entire large intestine.
In HD the ganglion cells are missing from the bowel. Contents are pushed along until they reach the affected part of bowel where the passage slows and a blockage occurs.
There is normally a delay in the baby passing meconium (black sticky stool normally passed within 24 hours of delivery).
Many babies with HD present at around three days of age having never had their bowels open. Baby may be reluctant to feed and may vomit a green fluid called bile which would normally pass through the bowel.
The abdomen (tummy) becomes distended. Sometimes the bowels become inflamed and a very serious infection called enterocolitis can develop.
- Milk feeds will be stopped.
- A tube will be passed through the nose into the stomach to drain away any fluid and air collecting in it.
- Fluids will be given through a vein (drip).
- Baby will need to have washouts to decompress the bowel and reduce discomfort. Usually the washouts will need to be done once or twice every day and will take 20-30 minutes.
Bowel washouts empty the lower large bowel of air and stool and reduce the risk of enterocolitis developing. Occasionally the abdomen cannot be decompressed adequately by washouts. Your baby would then need an operation (colostomy formation) to ensure that the bowel remains decompressed.
An X-ray of the baby’s abdomen will show dilated bowels. A dye study is done to see transition between dilated and narrow bowel. The only way to test the baby for HD is by taking a sample of tissue from the lining of the rectum through the baby’s bottom. This is called a Rectal Biopsy. The sample is sent to the laboratory for examination under a microscope. The results will be available in approximately five working days.
Bowel washouts are continued while waiting for the results of the rectal suction biopsy. They will be continued if HD is confirmed until the major operation for HD is performed.
Enterocolitis is an infection of the large bowel and is a potentially very serious complication of HD. It is treated with antibiotics (given through a drip into a vein) and regular bowel washouts. Some babies who develop enterocolitis need to have a stoma formed.
This operation is called a ‘Pull through’ and is usually performed at a few weeks/months of age. It involves taking out the part of the bowel affected by HD and connecting the healthy bowel to the anus. Sometimes this can be done using a laparoscopic approach (keyhole surgery).
12. Meckel’s Diverticulum
It is an outpouching of a part of small intestine which may contain a different type of lining tissue than the one found normally in the small intestine.
Abdominal pain, sometimes associated with rectal bleeding or blackish stools, voimiting. It can mimic appendicitis.
Diagnosis requires a number of tests and sometimes can be diagnosed only during Surgery. A blood test, ultrasonography , nuclear scan, CT scans may be required.
The diverticulum has to be surgically removed and a division and reconnection of small intestine may or may not be needed depending on the size. This surgery can be done either by open method or by key hole surgery.
13. Intussusception
It occurs when a part of intestine telescopes into the adjacent intestine and gets stuck there.
Abdominal pain, blood in stools (like red currant jelly ) , vomiting, distension of tummy
A reduction is tried by putting a tube in the rectum and instilling saline or dye under pressure. If it works, nothing more is required. If it doesn’t work, A surgery will be required to resolve the obstruction.
14. Alimentary tract duplications
It is an extra sac or pouch present alongside the normal intestine which has all the characteristics of the intestine but is blind ending.
Abdominal pain, , vomiting, distension of tummy or antenatally diagnosed
A surgery will be required to remove the cyst which amy entail removing part of the intestine and stitching it back together.
15. Mesenteric and Omental Cysts
These are balloon like sacs present in the tummy near the intestine which slowly increase in size and may cause problems like pressure on the intestines, digestion problems, bleeding , obstruction etc.
These need surgical excision
16. Rectal polyps
They are outpouchings of the lining of rectum/ end of the large intestine
90% of polyps are present in the last 5 cm of the rectum , the rest are found in the large intestine.
They present with rectal bleeding after passage of stools.
They are diagnosed byfinger examination through anus or by a colonoscopy
Rectal polyps can be surgically removed through the anus itself while large intestinal polyps need to be removed by doing a colonoscopy.
17. Appendicitis
Appendicitis is inflammation of the appendix. This can be caused by an infection or blockage of the appendix. With a blockage, the appendix can become swollen and easily infected by bacteria. The swelling and infection can cause the appendix to rupture (burst). This results in peritonitis (infection inside the abdomen) or the formation of an abscess around the appendix.
Pain that starts near the belly button, then moves to the right side.
Fever. Vomiting. In a perforated/ruptured appendix these symptoms may be more diffuse and catastrophic.
The diagnosis of appendicitis can usually be made by examining your child and discussing their symptoms. Blood tests, an ultrasound or other investigations may be done if the diagnosis is less certain.
The best treatment of appendicitis is removal of the appendix. The operation may be done through a single incision over the appendix or by laparoscopy (‘key hole’ surgery). Antibiotics are given at the time of the operation to reduce the chance of infection.
Pediatric Hepatobiliary Surgery
- Biliary Atresia
- Choledochal cyst
- Pancreatitis
- Pseudocyst of Pancreas

1. Biliary Atresia
Biliary atresia is a rare disease of the liver that scars and blocks the bile ducts. Because the bile is unable to drain, it builds up in the liver and damages the liver.
Bile ducts are tubes inside and outside the liver which carry bile to the intestine. Bile is a green brown fluid that helps with digesting food.
The cause of biliary atresia is not known. Suggested causes include viral infections or an over-response of the body’s immune system.
Symptoms or signs of biliary atresia typically appear in the first two months of life. These may include:
- Jaundice – A yellow appearance of the skin and whites of the eyes (sclera) can be present in many newborn babies. In biliary atresia, this jaundice does not improve within 1 to 2 weeks.
- Urine –Increased bilirubin in the bloodstream can make the urine appear very dark yellow or brown.
- Stools – Because bile and bilirubin does not reach the intestine, the stools can appear pale or clay-coloured.
Several other liver diseases can give the same symptoms as biliary atresia. Therefore a series of tests are needed to work out the cause of these symptoms. These tests include blood tests, urine tests, an ultrasound scan of the liver, tests to look at flow of bile through the liver (nuclear medicine scan or cholangiogram) and tests to look directly at the liver tissue (a biopsy). Biliary atresia is usually diagnosed after checking the results of many of these tests.
Babies with biliary atresia need surgery. Usually an operation called a portoenterostomy (sometimes called a Kasai procedure) is performed. This operation involves removing the blocked ducts and connecting the liver directly to the small intestine so that bile may be able to drain away from the liver.
An early operation can improve the outcome of biliary atresia. About 25% of infants will have good bile flow after surgery while 50% will have some bile flow. The remaining 25% will have little or no bile flow and the only option then is liver transplantation. Some infants initially improve but then continue to develop worsening liver disease and need liver transplantation. All infants who have biliary atresia need to be monitored closely by specialist doctors and teams through childhood, even if they are doing well. Biliary atresia is the most common reason for liver transplantation in children.
- Cholangitis – This is an infection of the tiny bile ducts in the liver caused by bacteria moving up from the bowel into the liver. It is a common problem after the Kasai procedure and can be life threatening as infants can become very sick very quickly. Symptoms include irritability, fever, increased jaundice and poor appetite. Any child who has had a Kasai procedure who develops any of these symptoms needs to seek medical treatment. Cholangitis is treated with intravenous antibiotics in hospital.
- Failure to thrive – Bile is needed for fat digestion in the intestine. So poor bile drainage results in poor growth and deficiency of certain vitamins. Vitamins A, D, E and K can be given orally to prevent deficiencies of these vitamins.
- Cirrhosis – This is scarring of the liver that results from long term damage. Cirrhosis itself can also impair growth and physical development of the child.
- Portal hypertension – As the liver becomes scarred, blood vessels travelling through the liver become constricted. This impairs the flow of blood and increases the pressure in these veins, specifically in the portal vein (a major vein of the liver system). Increased pressure in the veins connected to the portal vein lead to an enlarged spleen and possibly to ascites or varices (see below).
- Ascites – Excess fluid in the abdominal cavity which can cause the child’s tummy to be enlarged.
- Varices – These are swollen veins in the gastrointestinal tract that form due to portal hypertension. Varices can lead to bleeding. This bleeding can cause dark or black-coloured stools and blood-stained vomit. If this occurs, the child should be taken to the nearest hospital immediately.
Useful Websites
Liver Kids Organisation www.liverkids.org.au
Children’s Liver Disease Foundation (UK) www.childliverdisease.org
Children’s Liver Association for Support Services (USA) www.classkids.org
2. Choledochal cyst
Choledochal cysts, are rare congenital dilations (enlargements) of the bile ducts, a network of long tube-like structures that carry bile from the liver to small intestine for digestion.
Choledochal cysts are classified into 5 types, based on site of the cyst or dilatation.
- Type I: Most common variety (80-90%) involving saccular or fusiform dilatation of a portion or entire common bile duct (CBD) with normal intrahepatic duct.
- Type II: Isolated diverticulum protruding from the CBD.
- Type III or Choledochocele: Arise from dilatation of duodenal portion of CBD or where pancreatic duct meets.
- Type IVa: Characterized by multiple dilatations of the intrahepatic and extrahepatic biliary tree.
- Type IVb: Multiple dilatations involving only the extrahepatic bile ducts.
- Type V or Caroli’s disease: Cystic dilatation of intra hepatic biliary ducts
Although choledochal cysts are present at birth, they are diagnosed a little later in life.Symptoms may include:
- Jaundice – A yellow appearance of the skin and whites of the eyes (sclera)
- Urine –Increased bilirubin in the bloodstream can make the urine appear very dark yellow or brown.
- Stools –They may vary between yellow at times to pale or clay-coloured at other times.
Choledochal cysts are inflammatory in nature. Left untreated, this frequently lead to recurrent cholangitis (inflammation and infection in the bile ducts) or pancreatitis (inflammation of the pancreas).
Bile duct surgery with total cyst removal is the definitive treatment for choledochal cysts. This is followed
by reconstruction of the biliary tree with hepaticojejunostomy (connection between bile duct and intestine). Future complications include cholangitis( infection of bile ducts) and a 2% risk of cancer, which may develop in any part of the biliary tree.
3. Pancreatitis
4. Pseudocyst of Pancreas
PEDIATRIC UROLOGY
- Meatal stenosis
- Urethral duplication
- Ureterocele
- Bladder exstrophy

Pediatric Oncosurgery
Kidney tumours
Adrenal gland tumours
Liver tumours
Gastrointestinal tumours

